- term pilon (hammer) fracture was introduced to describe these compression injuries by Destot in 1911;
- ref: High-energy tibial pilon fractures: an instructional review.
- frx components:
- combination of ankle frx & distal tibial metaphyseal frx, usually w/ intra articular comminution;
- frx of medial malleolus;
- frx of anterior margin of tibia;
- transverse frx of posterior tibial surface;
- 20-25% of these will be open;
- mechanism of injury:
- vertical loading drives talus into distal tibia;
- position of foot & rate of loading affect injury pattern;
- it is important to distinguish between low energy frx (from skiing) vs high energy frx (as from MVA);
- plantar flexion: posterior articular damage;
- dorsiflexion: anterior articular damage;
- fibular frx:
- if fibula is frxed, then force involved is usually valgus shear w/ severe injury to the lateral aspect of the joint;
- fibula intact: (25% of injuries);
- pilon frx w/o assoc frx of fibula occur in approx 15 % of cases;
- w/ compression injuries fibula may remain intact, which never happens w/ shearing type injury;
- w/ intact fibula, ankle is often driven into varus w/ severe impaction of the medial part of the tibial plafond;
- associated injuries: (30% will have ipsilateral injuries and 5-10% will have bilateral injuries;)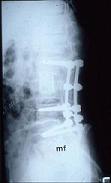
- compartment syndrome
- Acute compartment syndrome of the foot following fixation of a pilon variant ankle fracture
- compression frx of vertebral column, particularly L1;
- contralateral fractures of: os calcis, tibial plateau, pelvis, or acetabulum (verticle shear injuries):
- vascular injuries:
- Vascular abnormalities as assessed with CT angiography in high-energy tibial plafond fractures.
- outomes:
- with operative treatment, high energy pilon fractures will take 4 months on average to heal;
- 75% of patients who do not develop wound complications may expect a good result;
- subsequent arthrodesis rate may be as high as 10%;
- large number of patients will have pain even after 2 years post injury;
- references:
- Tibial Plafond Fractures. How Do These Ankles Function Over Time?
- Outcomes After Treatment of High-Energy Tibial Plafond Fractures.
- Outcome Following Open Reduction and Internal Fixation of Open Pilon Fractures
- The Sequential Recovery of Health Status after Tibial Plafond Fractures
 - Exam:
- Exam:
- soft tissue: note presence of swelling and any fracture blisters;
- perform an Allen test using a pulse oximeter for the foot vasculature (pulse ox is placed on the toe);
- note function of posterior tibial pulse while the dorsalis pedis pulse is occluded and vice versa;
- ideally, the pulse ox should demonstrate normal mp3e forms even w/ occlusion of either vessel;
- reference: The management of the soft tissues in pilon fractures.
- Radiographs: 
- consider a traction x-rays of extremity to help judge effects of ligamentotaxis on displaced articular fragments;
- CT scan: helps plan surgical fixation of articular fragments;
- note whether fibula is intact or fractured;
- w/ comminuted fibular fracture it is important to bring fibula out to length (talo-crural angle)
- w/ fibula intact, carefully evalute the syndesmosis;
- classification: and degree of articular comminution;
- type I: pilon frx
- type II: pilon frx
- type III: pilon frx
- type A:
- minimal or no anterior tibial cortical communition, two or more large tibial articular fragments,
and usually an oblique or transverse fibular fracture at level of the plafond (or ankle joint);
- type B:
- results from severe axial compression force, causing distal tibial bony impaction and comminution;
- Surgical Treatment:
- controversies:
- surgical timing and staged reconstruction;
- plate vs ex fix;
- ankle arthrodesis;
- primary arthrodesis is one consideration with severe injuries;
- references:
- Ankle arthrodesis using antegrade intramedullary nail for salvage of nonreconstructable tibial pilon fractures.
- Fracture reduction and primary ankle arthrodesis: a reliable approach for severely comminuted tibial pilon fracture.
- Primary Arthrodesis of the Tibiotalar Joint in Severely Comminuted High-Energy Pilon Fractures.
- initial treatment and timing of surgery
- current thinking: external fixation (with or without fibular fixation) followed by delayed definitive fixation at 12-24 days;
- Does a staged posterior approach have a negative effect on OTA- 43C fracture outcomes?
- Clinical and radiographic outcomes in patients operated for complex open tibial pilon fractures.
- Surgical Fracture Fixation: surgical technique:
- reduction and ORIF of fibula;
- exposure of tibial articular surface
- restoration of tibial articular surface
- Treatment of AO/OTA 43-C3 Pilon Fracture: Be Aware of Posterior Column Malreduction.
- fixation of metaphysis to diaphysis:
- Risk Factors for Tibial Plafond Nonunion: Medial Column Fixation May Reduce Nonunion Rates.
- Implants:
- plate fixation
- IM Nail: (see Nail fixation of distal tibia)
- references:
- Is there a role for intramedullary nails in treatment of simple pilon fractures? Rationale and preliminary results.
- Intramedullary Nailing in a Tibial Shaft Fracture With Distal Articular Extension
- Distal metaphyseal fractures of the tibia with minimal involvement of the ankle. Classification and treatment by locked intramedullary nailing..
- [Combination of intramedullary nail and covered screw osteosynthesis for managing distal tibial fracture with ankle joint involvement].
- Extra-articular distal tibia fractures: a mechanical evaluation of 4 different treatment methods.
- Intramedullary nailing of unstable diaphyseal fractures of the tibia with distal intraarticular involvement.
- uniplanar external fixation
- external fixation - foot inclusion
- circular wire fixators
- theoretically, there is some danger of osteomyelitis in having transfixation wires pass through the fracture segments
since incidence of pin tract infections in pilon fractures may be as high as 55%;
- other complications with circular wire fixators include ankle stiffness, swelling, RSD, and ankle tendon injury;
- references:
- Treatment of displaced pylon fractures with circular external fixators of Ilizarov.
- External Fixation Versus ORIF for Distal Intra-articular Tibia Fractures.
- cancellous bone grafting of metaphyseal defect
- wound closure:
- ref: The management of the soft tissues in pilon fractures.
- Complications:
- wound complications and infection: (see soft tissue coverage for tibia fracture)
- w/ tranditional early ORIF of the tibial articular surface the occurrance of wound slough and infection
has ranged from 10 to 50%;
- some feel that this complication can be minimized by delayed ORIF (once the swelling has diminish
 ed);
ed);
- 37% deep infection rate in tibial plafond Rüedi III (Teeny and Wiss (1993));
- unplanned surgery for complications (Wyrsch (1996))
- 55% for ORIF
- 18% for external fixation and limited ORIF
- degenerative joint disease:
- rates for secondary ankle arthrodesis after attempted ORIF of type 3 fractures approaches 30%.
- syndesmotic injuries:
- Syndesmosis and Syndesmotic Equivalent Injuries in Tibial Plafond Fractures.
- references:
- Open reduction and internal fixation of tibial plafond fractures. Variables contributing to poor results and complications.
- Complications encountered in the treatment of pilon fractures.
- Delayed wound healing, infection, and nonunion following open reduction and internal fixation of the tibial plafond fractures.
- The management of the soft tissues in pilon fractures.
- Early complications following the operative treatment of pilon fractures with and without diabetes.
- Operative Treatment of Fractures of the Tibial Plafond. A randomized, prospective study
The treatment of displaced fractures at the ankle by rigid internal fixation and early joint movement.
Fractures of the tibial pilon.
Intraarticular "pilon" fracture of the tibia.
Pylon fractures of the distal tibia.
Pilon fractures of the tibia: a study based on 19 cases.
Fractures of the tibial plafond. Evolving treatment concepts for the pilon fracture.
Tibial pilon fractures: a comparative clinical study of management techniques and results.