- Discussion: 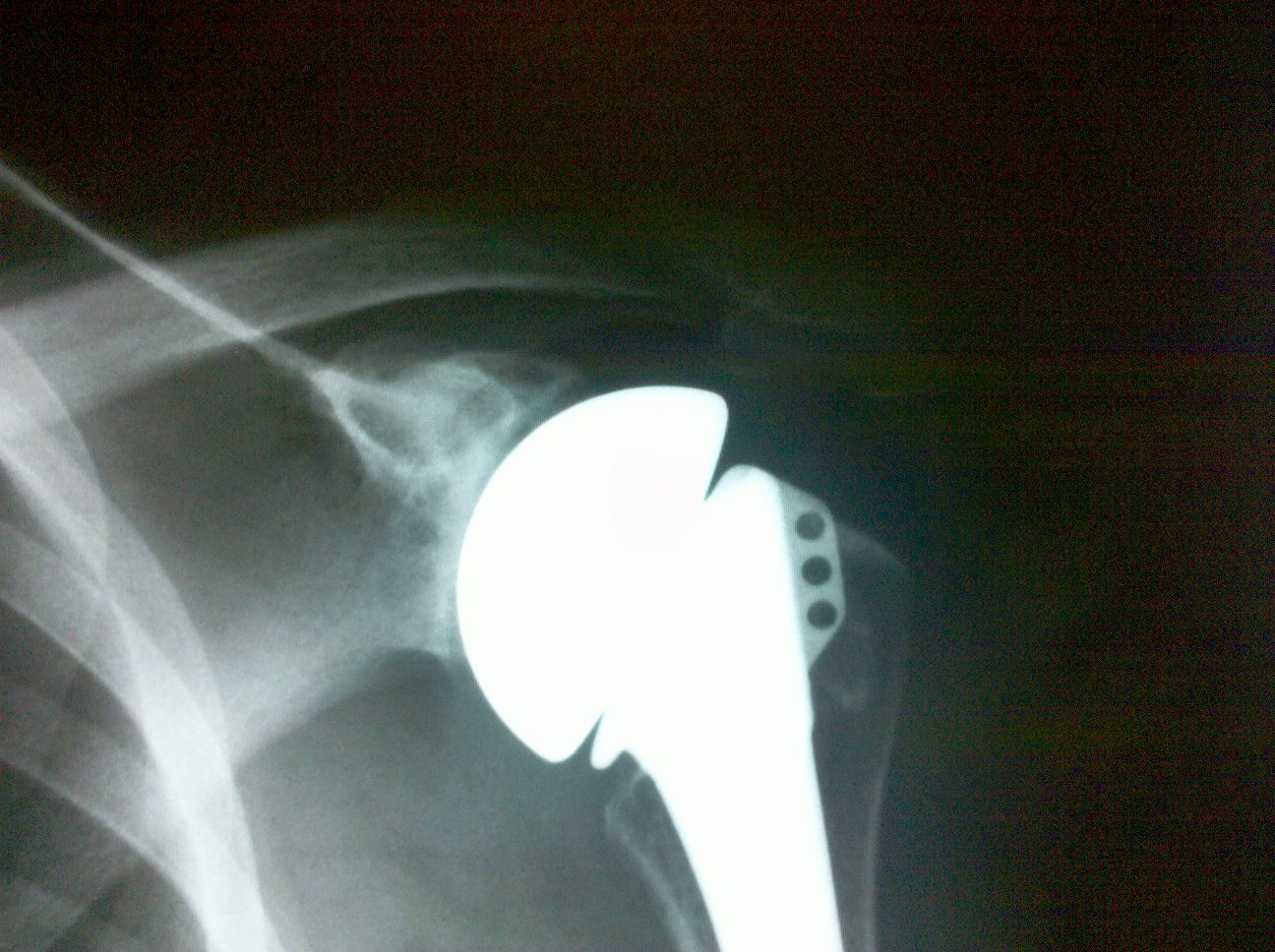
- see discussion shoulder arthroplasty and technical considerations with fracture
- operative considerations: hemiarthroplasty vs total shoulder arthroplasty
- considered in young pt w/ OA, posttraumatic dz (w/ no have glenoid involvement nor erosion), AVN, or massive RTC tear;
- approximate survival rate at 10 years is about 80%;
- need for revision is significantly higher in patients who underwent hemiarthoplasty for trauma rather than for RA;
- up to one half of younger patients undergoing hemiarthroplasty will have subjective or objective unsatisfactory results;
- complications unique to shoulder hemiarthroplasty include erosion of the glenoid which may eventually occur in upto 70% of patients;
- of patients undergoing revision hemiarthroplasty, the vast majority will be performed for a painful glenoid arthritis;
- indications / inclusion criteria: (for hemiarthroplasty instead of total shoulder arthroplasty);
- concentric glenoid consisting of eburnated bone
- humeral head needs to be centered in the glenoid preoperatively or at the time of surgery;
- there needs to be less than 25% intraoperative subluxation of the trial humeral component, after soft tissue balancing;
- non concentric glenoid: hemiarthroplasty may still be indicated if the glenoid can be converted to a smooth concentric surface w/ reaming;
- reference:
- Treatment of Glenohumeral Arthritis with a Hemiarthroplasty: A Minimum Five-Year Follow-up Outcome Study.
- Surgical Technique
- humeral component preparation and insertion:
- modular head
- note that in choosing a hemiarthroplasty component, it may be useful to select one with a modular head, so that the head can be removed if a
future glenoid resurfacing procedure is required;
- if the head is not modular, then the entire stem would have to be removed inorder to achieve the necessary exposure for glenoid arthroplasty;
- biologic glenoid resurfacing
- Humeral Hemiarthroplasty with Biologic Resurfacing of the Glenoid for Glenohumeral Arthritis. Two- to fifteen-year outcomes
- Nonprosthetic glenoid arthroplasty with humeral hemiarthroplasty and TSA yield similar outcomes in management of comparable patients with glenohumeral arthritis
- RESURFACED BUT NOT REPLACED – GLENOID TREATMENT FOR SHOULDER RESURFACING ARTHROPLASTY
- references:
- Acute prosthetic replacement for severe fractures of the proximal humerus.
- Modular hemiarthroplasty for fractures of the proximal part of the humerus.
- Bipolar implant shoulder arthroplasty. Long-term results.
- Total shoulder arthroplasty versus hemiarthroplasty. Indications for glenoid resurfacing.
- Prosthetic replacement of the proximal humerus.
- Glenoid loosening in total shoulder arthroplasty. Associaton with rotator cuff deficiency.
- Bipolar hemiarthroplasty for chronic rotator cuff tear arthropathy
- Optimizing the Glenoid Contribution to the Stability of a Humeral Hemiarthroplasty without a Prosthetic Glenoid.
- Humeral Head Replacement for the Treatment of Osteoarthritis.
- see discussion shoulder arthroplasty and technical considerations with fracture
- operative considerations: hemiarthroplasty vs total shoulder arthroplasty
- considered in young pt w/ OA, posttraumatic dz (w/ no have glenoid involvement nor erosion), AVN, or massive RTC tear;
- approximate survival rate at 10 years is about 80%;
- need for revision is significantly higher in patients who underwent hemiarthoplasty for trauma rather than for RA;
- up to one half of younger patients undergoing hemiarthroplasty will have subjective or objective unsatisfactory results;
- complications unique to shoulder hemiarthroplasty include erosion of the glenoid which may eventually occur in upto 70% of patients;
- of patients undergoing revision hemiarthroplasty, the vast majority will be performed for a painful glenoid arthritis;
- indications / inclusion criteria: (for hemiarthroplasty instead of total shoulder arthroplasty);
- concentric glenoid consisting of eburnated bone
- humeral head needs to be centered in the glenoid preoperatively or at the time of surgery;
- there needs to be less than 25% intraoperative subluxation of the trial humeral component, after soft tissue balancing;
- non concentric glenoid: hemiarthroplasty may still be indicated if the glenoid can be converted to a smooth concentric surface w/ reaming;
- reference:
- Treatment of Glenohumeral Arthritis with a Hemiarthroplasty: A Minimum Five-Year Follow-up Outcome Study.
- Surgical Technique
- humeral component preparation and insertion:
- modular head
- note that in choosing a hemiarthroplasty component, it may be useful to select one with a modular head, so that the head can be removed if a
future glenoid resurfacing procedure is required;
- if the head is not modular, then the entire stem would have to be removed inorder to achieve the necessary exposure for glenoid arthroplasty;
- biologic glenoid resurfacing
- Humeral Hemiarthroplasty with Biologic Resurfacing of the Glenoid for Glenohumeral Arthritis. Two- to fifteen-year outcomes
- Nonprosthetic glenoid arthroplasty with humeral hemiarthroplasty and TSA yield similar outcomes in management of comparable patients with glenohumeral arthritis
- RESURFACED BUT NOT REPLACED – GLENOID TREATMENT FOR SHOULDER RESURFACING ARTHROPLASTY
- references:
- Acute prosthetic replacement for severe fractures of the proximal humerus.
- Modular hemiarthroplasty for fractures of the proximal part of the humerus.
- Bipolar implant shoulder arthroplasty. Long-term results.
- Total shoulder arthroplasty versus hemiarthroplasty. Indications for glenoid resurfacing.
- Prosthetic replacement of the proximal humerus.
- Glenoid loosening in total shoulder arthroplasty. Associaton with rotator cuff deficiency.
- Bipolar hemiarthroplasty for chronic rotator cuff tear arthropathy
- Optimizing the Glenoid Contribution to the Stability of a Humeral Hemiarthroplasty without a Prosthetic Glenoid.
- Humeral Head Replacement for the Treatment of Osteoarthritis.

