- See: Acetabular Component Menu 

Discussion
- it is controversial as to whether screws are necessary in THR, and there are relative advantages and disadvantages;
- cups should be designed with only 2-3 holes so as to maximize the porous coating surface and to minimize conduit for osteolysis;
- acetabular cup insertion:
- advantages of screw insertion:
- theoretically, screw fixation can close any gap created by non congrous reaming;
- prevents the loss of compressive stresses and resultant shear stresses;
- may be indicated in osteoporotic bone (when insertion of over-sized components may not be wise) and when additional fixation is required;
- screw insertion is also indicated in situations in which there is insufficient bony coverage;
- biomechanical considerations: (design of components)
- references:
- Micromotion of cementless hemispherical acetabular components. Does press-fit need adjunctive screw fixation?
- The relation between micromotion and screw fixation in acetabular cup.
- The number of screws, bone quality, and friction coefficient affect acetabular cup stability
- Cementless acetabular fixation with and without screws: analysis of stability and migration.
- references:
- controversies: Do acetabular screws promote osteolysis?
- although screws may provide excellent initial fixation, later they may be sources of fretting, which could produce wear debris, and provide a conduit for migration of the polyethylene debris;
- in order to reduce the chance of osteolysis some surgeons insert the least number of screws possible in order to achieve solid fixation;
- while screws may provide a conduit for wear debris, unfilled screw-holes may also provide access for wear debris from ultra-high molecular weight polyethylene liner to area behind ingrowth cup;
- ultra-high molecular weight polyethylene may cold-flow (creep) into these holes, resulting in early failure of the polyethylene liner;
- hence, it remains unclear as to whether screws strongly influence the formation of osteolysis in acetabular components which contain screw holes;
- Dorr et al 1998 and by Latimer 1996, there is a paucity of evidence to support notion that screw fixation leads to osteolysis;
- certainly, if a screw does not achieve a rigid bite it should be removed - due to the risk of osteolysis;
Radiographic Evaluation of Screw Position
- Judet views;
- references:
Screw Placement Considerations
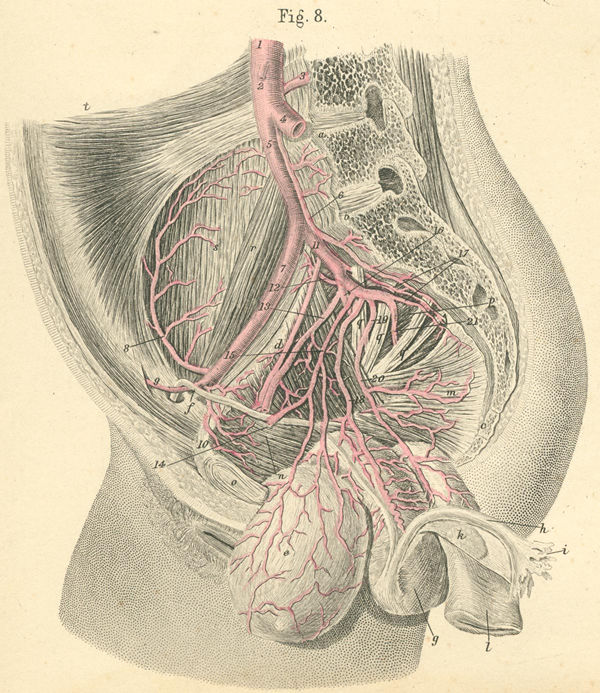
- main issue is to avoid vascular injuries:
- note that a relatively retroverted, vertically inserted cup will be at most risk for neurovascular injury;
- hence, an optimally anteverted and positioned acetabular component will have the least risk of injury;
- when in question, screws aimed just anterior to the sciatic notch, will find safe passage in strong bone;
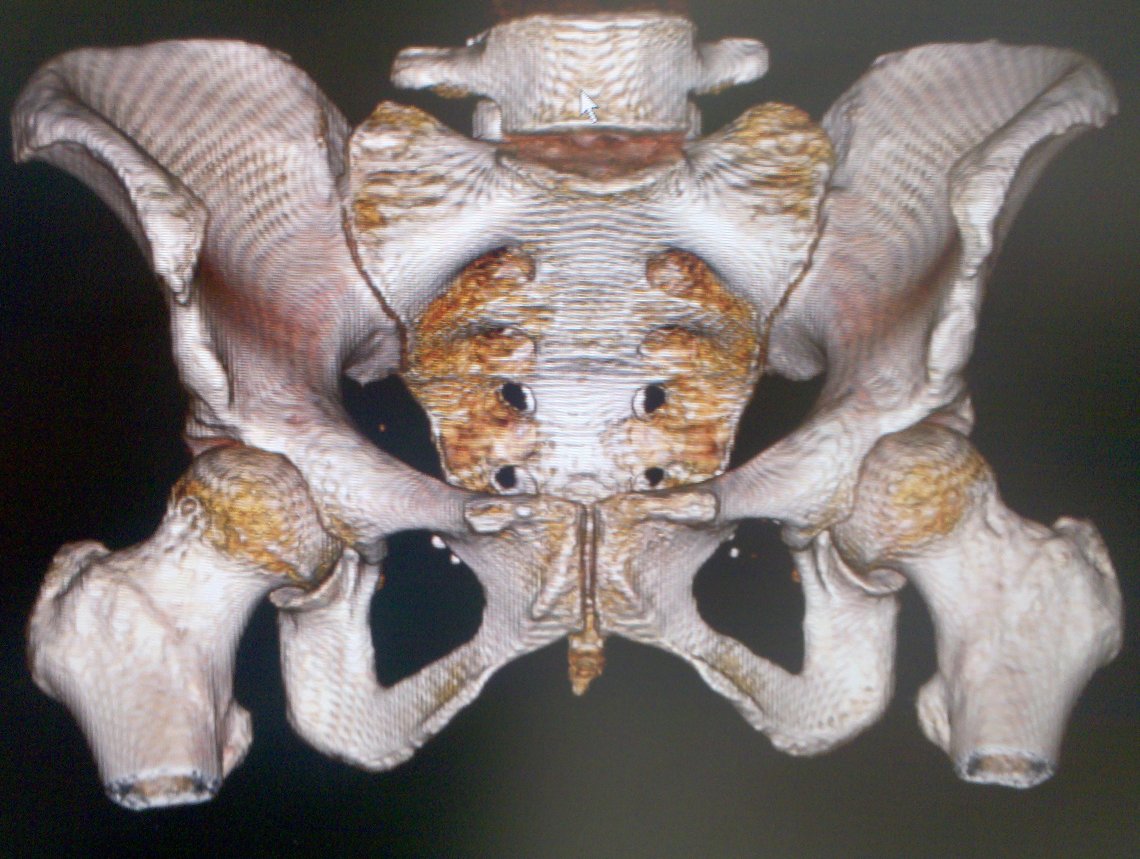
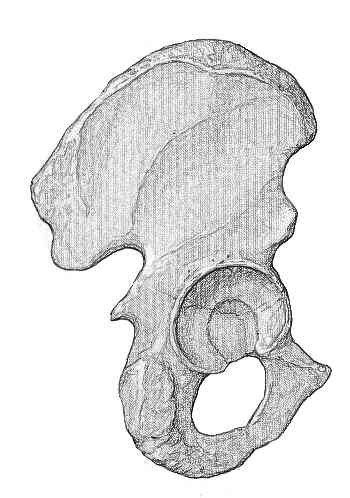
- quadrant system:
- based on line from ASIS through center of acetabulum;
- safe quadrant is defined by two lines from the anterior-inferior iliac spine through the center of the acetabulum and posterior by a line from the sciatic notch to the center of the acetabulum;
- screws placed thru posterosuperior & posteroinferior quadrants do not emerge within the pelvis;
- posterosuperior quadrant is the safest;
- in posterosuperior quad, screws > 25 mm frequently are placed thru strong bone in this area (bone around sciatic notch is especially strong);
- usually do not need screws greater than 35 mm long are placed in the posterosuperior quadrant
- screws may pass into sciatic notch and endanger sciatic nerve and superior gluteal vessels;
- protect sciatic nerve durig placement of screws, w/ finger along sciatic notch to prevent penetration of drill or screw;
- fixation of screws placed posterosuperiorly may be achieved without drilling through the second cortex, bicortical fixation is usually unnecessary;
- with osteoporotic bone, firm fixation of screws placed superiorly often requires that the screws reach proximally enough to contact both cortices;
- avoid bicortical screw placement with patients on anticoagulants;
- posteroinferior quadrant:
- in posteroinferior quad, screws are rarely longer than 20-25 mm;
- need to ensure that screw does not impale sciatic nerve;
- ref: Does ischial screw fixation improve mechanical stability in revision total hip arthroplasty?
- anterior-superior quadrant:
- external iliac vein is most at risk w/ anterosuperior screws, but the iliac artery may be damaged as well;
- located within 7 mm of the anterior column of the pelvis at the anterior inferior iliac spine and within 4 mm at the acetabular dome;
- external iliac artery: within 10 mm of the bone at the anterior inferior iliac spine and within 7 mm at the acetabular dome
- references:
- external iliac vein is most at risk w/ anterosuperior screws, but the iliac artery may be damaged as well;
- anterior-inferior quadrant:
- obturator artery is most at risk with anteroinferior screws;
- screws may injure obturator nerve, artery, and vein;
- quadrilateral surface: interposition of the obturator internus muscle between the obturator vessels;
Other Considerations
- if drill holes are placed eccentrically, then screw insertion may lift cup up out of the bony bed;
- screw heads left pround wont allow liner to be fully seated
Complications
- vascular injuries:
- most common injuries include: external iliac artery, common femoral artery, external iliac vein;
- occurs more commonly in females and in the left hip;
- references:
- Vascular injury during total hip arthroplasty: the anatomy of the acetabulum
- External iliac vein compression and thrombosis by a migrated acetabular screw following total hip arthroplasty
- Retroperitoneal hematoma with bone resorption around the acetabular component after total hip arthroplasty: a case report and review of the literature
- Current overview of neurovascular structures in hip arthroplasty: anatomy, preoperative evaluation, approaches, and operative techniques to avoid complications.
- Internal iliac artery injury and total hip arthroplasty: discovery after 10 years.
- Evaluation of intra-pelvic screw position prior to revision total arthroplasty--a report of 2 cases.
- THA With Acetabular Fixation: An Unexpected Complication
- An unusual cause of Grey Turner's sign.
- visceral injuries:
References:
- Neurovascular Injuries in Acetabular Reconstruction Cage Surgery. An Anatomical Study.
- L5 Radiculopathy Secondary to Intrapelvic Placement of Acetabular Cup Fixation Screw
- Structures at risk from medially placed acetabular screws.
- Acetabular anatomy and transacetabular screw fixation at the high hip center
- Safe Zone for Transacetabular Screw Fixation in Prosthetic Acetabular Reconstruction of High Developmental Dysplasia of the Hip.
- The relationship of the intrapelvic vasculature to the acetabulum. Implications in screw-fixation acetabular components.
- Acetabular anatomy and the transacetabular fixation of screws in total hip arthroplasty.
- Screw Augmentation: the gold standard for cementless cup fixation.
- The relation between micromotion and screw fixation in acetabular cup
- Screw-augmented fixation of acetabular components. A mechanical model to determine optimal screw placement.
- [The anatomical study of safe zones of the screw fixations in acetabular revision surgery].
- Anatomic Assessment of the Acetabular Fossa for Screw Fixation in Acetabular Fracture
- Current Overview of Neurovascular Structures in Hip Arthroplasty: Anatomy, Preoperative Evaluation, Approaches, and Operative Techniques to Avoid Complications.