- Discussion: Tibial Plateau Frx Menu
- lateral plateau frxs include:
- type I fractures
- type II fractures
- type III fractures
- local compression frx which are similar to type iii frx
- Surgical Stratedgy:
- extensile surgical approach that exposes whole frx zone & adjacent normal tissue;
- comminuted type II fractures will often require more extensive exposure than type I fractures, however, in both cases, "booking open" the fracture
site will yield exellent access to the entire lateral compartment;
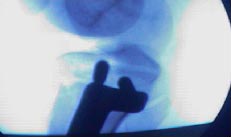
- fixation strategy involves ORIF of comminuted articular surface w/ subchondral reduction & buttressing of split frag that forms lateral wall;
- PreOp Planning (positioning, and implants);
- w/ significant frx shortening (and resultant valgus) consider using AO large distractor & relying on ligamentotaxis to maintain reduction and provide exposure;
- usually is distractor is placed on the same side as the frx;
- one pin is inserted into the femoral condyle and one in the mide tibia;
- supine position:
- tape a rolled sheet onto table (as with a total knee replacement), in order to allow the knee to remain hyperflexed during procedure (when required);
- supine w/ leg flexed:
- leg can be positioned as for arthroscopy;
- a leg holder is applied to the proximal thigh, and the table is broken to allow the knee to flex past 90 deg;
- the opposite leg is then held in a GYN leg holder;
- this technique allows varus to be applied to the knee which improves fracture exposure;
- Limited Hockey Stick Incision:
- most useful in situations where only cannulated screws will be used (and plate butressing is not required);
- if butressing is necessary, consider external fixation (circular frame fixation);
- statedgy involves booking open fracture site which yields excellent exposure of lateral compartment, especially if arthroscopy is used (placed underneath meniscus);
- this approach is also especially useful w/ concomitant meniscal tears;
- this incision should not interfere w/ total knee incision (should it be necessary in the future);
- technique: (see: lateral capsular anatomy of the knee);
- incision is made from a point above the fibular head to Gerdy's tubercle;
- it can be biased either anteriorly or posteriorly to lie directly over the fracture;
- carry the dissection directly down to the IT band, and then palpate the anterior frx line;
- split the IT band in line with its fibers directly over the fracture site;
- fracture site and the joint capsule are now visible;
- just below joint line, make a horizontal inframeniscal incision, which extends from a point anterior to frx fragment to a point posterior to frx fragment;
- infra-meniscal incision needs to be large enough to allow the meniscus to be elevated and the frx to be "booked open";
- once the split fragment is booked open, there should be excellent access to the compartment;
- Longitudinal Incision:
- most indicated when a butress plate is required;
- this approach will not interfere w/ a TKR incision if one is needed in the future;
- slightly lateral parapatellar (or midline incision) is made from about 10 cm above the patella to about 3-4 cm below the lowest extent of the frx;
- incision is carried directly down to the superificial retinaculum, and a full thickness flap is elevated once underneath the superficial retinaculum;
- the flap is mobilized laterally and distally, so that with the knee flexed Gerdy's tuberlce is exposed;
- deep dissection: (see: lateral capsular anatomy of the knee);
- most important step in reconstruction of any intra articular frx, is to expose fracture w/o devasclarizing the fragments;
- flex the knee to 90 deg, and incise thru the IT band (along its fibers) directly over the split frx site;
- Anterior Meniscal Detachment: 
- see: lateral meniscus;
- just below the joint line, make a horizontal inframeniscal incision, which extends from a point anterior to the frx
fragment to a point posterior to the frx fragment;
- infra-meniscal incision needs to be large enough to allow the meniscus to be elevated and the frx to be "booked open";
- sharply detach the anterior horn of menisci from its bony insertion;
- the anterior horn will later be repaired at the end of the case;
- this allows the surgeon to pull up on meniscus together w/ the attached capsule, for more optimal view of articular surface;
- meniscus is retracted proximally, and the joint inspected directly;
- if the arthrotomy is made above the meniscus, the meniscus will keep most of articular surface hidden from view;
- the knee is hyperflexed and internally rotated;
- meniscal re-attachment:
- two small drill holes are made at the origin of the anterior horn and are directed to exit medial to the patellar tendon;
- pass a suture thru the meniscus, and use a suture passer to thread the sutures through the drill holes;
- references:
- Meniscal detachment to approach lateral tibial plateau fractures.
- The use of an anterior incision of the meniscus for exposure of tibial plateau fractures requiring open reduction and internal fixation.
- Meniscal detachment to approach lateral tibial plateau fractures.
- Alternative Extensile Measures:
- tubercle osteotomy:
- however, always avoid tubercle osteotomy in bicondylar frx since, this might be the only intact portion of bone anteriorly;
- if tibial tubercle is already fractured, then it may be detached - as would be in an osteotomy;
- patellar tendon Z-plasty:
- contra-indicated if there is concomitant tibial tubercle frx;
- for improved exposure, consider cutting the patella in a "Z pattern" (longitudinal split w/ half attach to tubercle and half
attached to patella) with repair of the tendon with heavy suture at the end of the case (see repair of patellar tendon rupture);
- in this technique, the adjacent parapatellar retinaculum should be left intact; 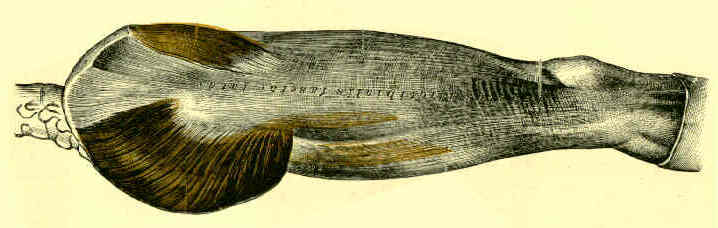
- wide IT band flap:
- a wide exposure is required for comminuted type II frx;
- knee is flexed to 90 deg, and the iliotibial band is retracted or split to expose midlateral capsule;
- incision is made thru the lateral 1/3 of the quadriceps, it is continued down along the lateral edge of the patella,
and is then continued down along lateral edge of the patella (incising the lateral retiancular expansion);
- the incision is continued distally below the frx line;
- 2nd deep capsular incision is made thru inferior 1/3 of IT band (crossing Gerdy's tubercle) which is split in line with
its fibers so that it intersects with the longitudinal capsular incision;
- alternatively capsular incision is carried below Gerdy's tuberlce, & tubercle is then detached w/ osteotome & IT band
is left attached to facilitate subsequent wound closure;
- this tongue of IT band and capsule is then elevated superiorly off the tibia, elevating the meniscus off the tibia in the process;
- this technique has been criticized for devascularizing the frx fragment;
- Reduction:
- knee is stressed into varus position for visualization of lateral plateau;
- if a depressed split fracture is difficult to reduce, consider application of a universal distractor to assist w/ the reduction;
- further periosteal stripping may be necessary to assist w/ reduction;
- staying w/in periosteal sleeve avoids damage to anterior tibial muscle and anterior tibial artery;
- depressed articular fragments are elevated with a punch, supported by bone graft, and buttressed with a lateral T or L shaped plate;
- k wire fixation:
- k wires are inserted to maintain provisional fixation;
- take care that k wire position does not interfere with plate application;
- bone graft that supports elevated fragments cannot hold them in anatomic relationship and is often secondarily depressed when patient starts ROM exercises;
- references:
- Evaluation of Popliteal Artery Injury Risk With Locked Lateral Plating of the Tibial Plateau
- The arterial vascularization of the lateral tibial condyle: anatomy and surgical applications.
- Anatomic location of the peroneal nerve at the level of the proximal aspect of the tibia: Gerdy's safe zone.



- Post Operative Care and Complications
A New Surgical Approach in the Treatment of Depressed Lateral Condylar Fractures of the Tibia.
A New Surgical Approach to Fractures of the Lateral Tibial Plateau.
Early weight bearing of lateral tibial plateau fractures.
A new posterolateral approach without fibula osteotomy for the treatment of tibial plateau fractures.
Posterolateral transfibular approach to tibial plateau fractures: technique, results, and rationale.
Combined Arthroscopic Treatment of Tibial Plateau and Intercondylar Eminence Avulsion Fractures


