- Technique:




- patient is placed on a bean bag in a true lateral position;
- slightly flexing the knee and placing it on a padded Mayo stand may facilitate positioning;
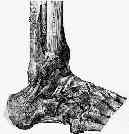
- calcaneus is approached thru an extensile right angled incision, which curves sharply between verticle and horizontal limbs;
- vertical limb
- made just anterior to achilles tendon & extends down to junction of plantar & lateral skin;
- the incision is posterior to the sural nerve;
- proximally, use a tonsil clamp to spread thru soft tissues to identify the sural nerve which is then tagged with a rubber damn;
- ensure vascularity of the flap:
- in the study by Borrelii and Lashgari (1999), it was found that the verticle limb of the incision is more likely
to endanger the delicate vascular anastomosis of the flap;
- these authors found three consistent arteries around the lateral aspect of the hindfoot (lateral calcaneal artery, lateral malleolar artery, and the lateral tarsal artery);
- these authors warn against placing the verticle limb too far anteriorly (or it will disrupt the lateral calcaneal artery);
- Vascularity of the lateral calcaneal flap: a cadaveric injection study.
- horizontal limb:
- extends horizontally at junction of plantar and lateral skin (glabrous junction) which also parallels inferior border of calcaneus;
- incision is carried forward and slightly upwards inorder to approach the calcaneo-cuboid joint;
- if the horizontal incision is made superior to the glabrous junction, the tissue between the incision and the glabrous junction may lie in a hypovascular which risks wound necrosis;
- develop full thickness flap;
- goal is to minimizes peroneal tendinitis & devascularization of anterior skin flap, & preserves sural nerve, which is within flap;
- at the apex of the incision, the knife is brought down directly to bone;
- more distally it is essential to also identify the sural nerve since the incision will always cross the nerve;
- one technique is to gently tug on the proximal sural nerve, inorder to help identify the distal sural nerve;
- peroneal tendon sheath is subperiosteally dissected from lateral malleolus until it is shifted anteriorly over malleolus as a unit;
- it is essential not to incise the peroneal retinaculum proximally, in order to avoid peroneal tendon subluxation;
- peroneal tendons are retracted anterior to fibula w/ 2 K wires, one in fibula and one in the talus (and perhaps one in the cuboid);
- calcaneofibular lig is identified & sharply cut off calcaneus & retracted anteriorly along w/ full thickness skin flap,
- wound closure:
- be sure to use a flap stitch with the knotted end on the other side of the flap (to minimize vascular damage)
Vascularity of the lateral calcaneal flap: a cadaveric injection study.

