- See:
- Malgaigne Fracture
- Sacral Fractures
- Sacroiliac Fracture Dislocations
- cresent fracture
- Evaluation of Stability:
- as noted by Kellam, et al. (1987), a stable injury is one that can withstand normal physiologic forces w/o excessive deformation;
- it is also noted, however, that there are some unstable posterior injuries that have a high potential for healing (sacral frx) and
others with a lower potential for healing (? somewhat similar to bony Chance frx);
- physical exam:
- evaluation under flouro:
- determine whether there is gross motion in any of the three planes (medial-lateral, AP, and cephalad-caudad) and determine
whether there is rotational instability;
- manual palpation may reveal a movable & therefore unstable hemipelvis, hemipelvic fragments were presumably partially
reduced in supine position, which is suspicious, but nondiagnostic, of pelvic instability;
- this group of pts may have only partial ligament damage;
- this group of pts may show displacement of x-rays on f/u films;
- ref: The unstable pelvic fracture. Operative treatment.
- Stability of Specific Injury Types:
- sacral frx:
- stable frx includes impacted vertical frx of sacrum, nondisplaced frx of posterior sacroiliac complex, and/or subtle frx of upper
sacrum as seen by asymmetry of sacral arcuate lines;
- unstable frx, is characterized by frx diastasis of more than 0.5 to 1 cm, along w/ an unstable anterior injury;
- vertical instability of hemipelvis: > 0.8 cm;
- caused by disruption of ventral sacroiliac, sacrospinous, & sacrotuberous ligaments as well as complete disruption of posterior
sacroiliac ligaments, w/ cephalad displacement of hemipelvis of > 0.5 to 0.8 cm;
- use outlet view for evaluation;
- anterior-posterior instability:
- disruption of ventral sacroiliac, sacrospinous, & sacrotuberous ligaments, & is represented by SI joint diastasis of > 1 cm;
- some consider diastatic frx of osseous components of posterior sacroiliac complex > 0.5 cm as unstable;
- note that an unstable frx may partially reduced in supine position;
- best seen on inlet view showing posterior displacement of sacrogluteal line, and is best confirmed by CT scan;
- rotational instability:
- lateral compression injury:
- unstable to internal rotation but is stable to external rotation (and actually reduces in external rotation);
- AP compression injuries:
- unstable to external rotation, but stable to internal rotation of the pelvis;
- rotational instability may be controled w/ external fixation;
- transverse process frx: (usually 5th lumbar);
- may be a minor sign of instability in about 20% of pts;
- even if these patients are found to have frx stability, many will have an ileus due to the severity of the trauma;
- anterior pelvic injury:
- generally pubic rami fractures will not require fixation followig fixation of the posterior pelvis, where as pubic
ramus disruption greater than 2.5 cm will require fixation;
- CT scan:
- useful in determining those whose initial x-ray appearance suspicious of instability and a clinical impression of stable pelvic
fracture;
- PreOp Planning:


- combined anterior & posterior unstable lesions:
- often cannot be approached simultaneously thru same incision, and rather it is necessary to stage the operation;
- in majority of cases, posterior lesion is approached first;
- following posterior internal fixation, an x-ray may show anterior reduction;
- w/ posterior injury + symphysis dislocation:
- symphysis dislocation may be reduced & fixed first if there are no associated fractures thru pubic rami or acetabulum;
- symphysis reduction may provide a partial reduction of pelvic ring followed by completion of reduction & fixation
posteriorly;
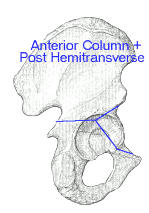
- combined posterior & unstable acetablar frx:
- reduction & internal fixation of posterior pelvic ring disruptions is performed prior to acetabular reduction whether posterior
ring disruption is ipsilateral or contralateral;
- pelvic ring distortion may make the acetabular frx impossible to reduce;
- type of acetabular frx may dictate surgical approach for posterior pelvic lesion;
- in case of SI dislocation assoc w/ anterior column frx both injuries are approached thru ilioinguinal approach;
- SI joint can be approached thru extended iliofemoral approach or by extending Kocher-Langenbeck approach;
- Choice of Incisions:
- choice of incision depends on assoc injuries, soft tissue contussion, abrasion, laceration, or hematoma cavities, as well as supra
pubic catheters;
- most posterior injuries can be assessed thru posterior surgical incision;
- posterior approach (Kocher Langenbock):
- anterior approach to SI joint:
- Choice of Hardware:
- orthomed pelvic reduction clamps
- percutaneous SI joint fixation
- indicated for sacroiliac fracture dislocations and for some sacral fractures;
- transiliac sacral bars:
- utilizes Harrington rods, w/ compression achieved by tightening of threaded nuts;
- advantages include technical ease of insertion and limited soft tissue dissection;
- relative contraindications include iliac wing fractures;
- cautions: may cause over compression of sacral fractures;
- see synthes technique guide
- 4.5 mm reconstruction plate: (Albert et al (1993))
- indicated for posterior pelvic fractures as well as sacral fractures;
- reconstruction plate is placed along dorsum of the sacral and thru the posterior iliac spines (transiliac plate fixation);
- advantages:
- low profile, minimal risk to N/V structures, and no need for flouro;
- patient is placed in the prone position;
- two incisions are made over the PSIS which are perpendicular to the iliac wings, and one vertical incision is made over the
base of the S1 spinous process;
- dissections are caarried down to the bony surfaces;
- predrill the PSIS to assist w/ reconstruction plate insertion;
- use the 4.5 drill to make 2-3 drill holes 1 cm lateral to the PSIS;
- an appropriately sized 4.5 mm reconstruction plate is chiseled thru the iliac spine, passed along the dorsum of the sacrum to
the opposite PSIS;
- the recon plate is appropriately contoured;
- the plate is fixed to the iliac wings using 6.5 mm cancellous screws, w/ two screws inserted into each ilac wing;
- postop: patients can be bed to chair or touch down wt bearing;
- ref:
- Posterior Pelvic Fixation Using a Transiliac 4.5 mm Reconstruction Plate: A clinical and biomechanical study.
General Orthopedics: A Tribute to J. Vernon Luck, Sr.--Symposium: Internal Fixation of Pelvic Ring Fractures.
Pelvic and Lower Extremity Trauma--Symposium: The Role of Standard Roentgenograms in the Evaluation of Instability of Pelvic Ring Disruption.
Advances in Greece--General Orthopaedics: Hip: Stabilization of Sacroiliac Joint Disruption With Threaded Compression Rods.
Posterior pelvic disruptions managed by the use of the Double Cobra Plate.
Anterior approach and stabilization of the disrupted sacroiliac joint.
Biomechanical testing of new and old fixation devices for vertical shear fractures of the pelvis.
Anatomy of the Posterior Iliac Crest as a Reference to Sacral Bar Insertion